May 2024
Choosing Walking Versus Running Shoes

When it comes to walking versus running, the distinction goes beyond just pace and intensity. As experts note, the mechanics of each activity necessitate specific footwear for walking and running. For walkers, shoes with soft, flexible soles are recommended to absorb the impact of each step and facilitate the rolling motion from heel to toe. Runners require thicker-soled shoes for ample shock absorption, given the varied striking points on the foot during a run. It is important to remember that while running shoes can serve for walking, the reverse is not recommended by experts. Footwear plays a critical role in preventing foot injuries like plantar fasciitis and Achilles tendonitis, but shoes alone cannot resolve existing issues. Seeking guidance from a podiatrist is essential if foot discomfort persists. To ensure the right shoe fit, have your arch and gait evaluated. For advice with foot pain related to either walking or running, it is suggested that you schedule an appointment with a podiatrist for a full exam and diagnosis. The appropriate treatment options will follow, including suggestions on the right type footwear for the activity.
For more information about walking shoes versus running shoes, consult with Gregory T. Loo, DPM from Elite Podiatry. Our doctor can measure your feet to determine what your needs are and help you find an appropriate pair of footwear.
Foot Health: The Differences between Walking & Running Shoes
There are great ways to stay in shape: running and walking are two great exercises to a healthy lifestyle. It is important to know that running shoes and walking shoes are not interchangeable. There is a key difference on how the feet hit the ground when someone is running or walking. This is why one should be aware that a shoe is designed differently for each activity.
You may be asking yourself what the real differences are between walking and running shoes and the answers may shock you.
Differences
Walking doesn’t involve as much stress or impact on the feet as running does. However, this doesn’t mean that you should be any less prepared. When you’re walking, you land on your heels and have your foot roll forward. This rolling motion requires additional support to the feet.
Flexibility – Walking shoes are designed to have soft, flexible soles. This allows the walker to push off easily with each step.
If you have any questions, please feel free to contact one of our offices located in Ahwatukee, and Phoenix, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Common Symptoms of Plantar Fasciitis
 Plantar fasciitis occurs when the thick band of tissue that runs along the bottom of your foot, called the plantar fascia, becomes inflamed. Plantar fasciitis is a common cause of heel pain. It is characterized primarily by a sharp, stabbing pain in the bottom of the foot near the heel. This pain is often more pronounced in the morning when taking the first steps of the day, or after long periods of sitting or standing. The pain may flare up with intense activity but typically worsens after, not during, the exercise. Other symptoms include swelling and tenderness in the heel area. Plantar fasciitis is particularly prevalent in runners, overweight individuals, and those whose jobs require long hours on their feet. Wearing shoes with inadequate support exacerbates the problem in those with plantar fasciitis. Effective treatment involves rest, stretching exercises, and proper footwear. If you have heel pain and suspect plantar fasciitis, it is suggested that you consult with a podiatrist, or foot doctor, for care.
Plantar fasciitis occurs when the thick band of tissue that runs along the bottom of your foot, called the plantar fascia, becomes inflamed. Plantar fasciitis is a common cause of heel pain. It is characterized primarily by a sharp, stabbing pain in the bottom of the foot near the heel. This pain is often more pronounced in the morning when taking the first steps of the day, or after long periods of sitting or standing. The pain may flare up with intense activity but typically worsens after, not during, the exercise. Other symptoms include swelling and tenderness in the heel area. Plantar fasciitis is particularly prevalent in runners, overweight individuals, and those whose jobs require long hours on their feet. Wearing shoes with inadequate support exacerbates the problem in those with plantar fasciitis. Effective treatment involves rest, stretching exercises, and proper footwear. If you have heel pain and suspect plantar fasciitis, it is suggested that you consult with a podiatrist, or foot doctor, for care.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Gregory T. Loo, DPM from Elite Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Ahwatukee, and Phoenix, AZ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes and Diagnosis of Peripheral Artery Disease
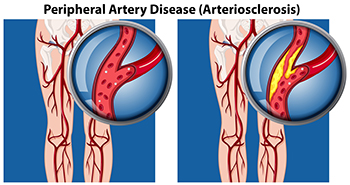
Peripheral artery disease, or PAD, poses significant challenges for foot health, stemming from restricted blood flow to the lower extremities. This condition, often caused by atherosclerosis, involves the buildup of fatty deposits in the arteries, leading to narrowed or blocked blood vessels. The diminished blood supply to the feet can result in various symptoms, including pain, cramping, numbness, and weakness, particularly during physical activity. Left untreated, PAD can contribute to serious complications such as foot ulcers, infections, and delayed wound healing. Diagnosing PAD typically involves a comprehensive evaluation by a podiatrist. This process includes a thorough medical history review, assessment of risk factors such as smoking and diabetes, and a physical examination focused on evaluating circulation in the legs and feet. Specialized diagnostic tests, such as ankle-brachial index, or ABI measurement, Doppler ultrasound, and angiography, may also be employed to confirm the diagnosis and determine the extent of arterial blockages. If you are experiencing any of the foot symptoms mentioned above, it is suggested that you consult a podiatrist who can accurately diagnose and offer relief solutions for PAD.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Gregory T. Loo, DPM from Elite Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Ahwatukee, and Phoenix, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes and Symptoms of Lisfranc Fractures

Lisfranc fractures or injuries, although rare, can be incredibly painful and often require prompt diagnosis and treatment. These injuries affect the joints in the middle of the foot, and while Lisfranc fractures can sometimes be mistaken for a sprain, they necessitate specialized care from a podiatrist. Causes include sports-related trauma, and everyday accidents like falling down stairs or having an object land on the foot. Among the symptoms are tenderness, swelling, bruising, and severe pain while standing or walking. Diagnosis typically involves a physical examination and X-rays, with further imaging like CT scans or MRIs sometimes necessary for surgical planning. In some cases, conservative treatment methods like immobilization with a cast or boot may suffice. In more severe cases, surgery may be prescribed, particularly if there are fractures, dislocations, or extensive soft tissue damage. If you are experiencing symptoms of a Lisfranc injury or have recently sustained an injury to your foot, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Gregory T. Loo, DPM from Elite Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact one of our offices located in Ahwatukee, and Phoenix, AZ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.